| Regeneration of Peripheral Nerve Axons after Damage | |
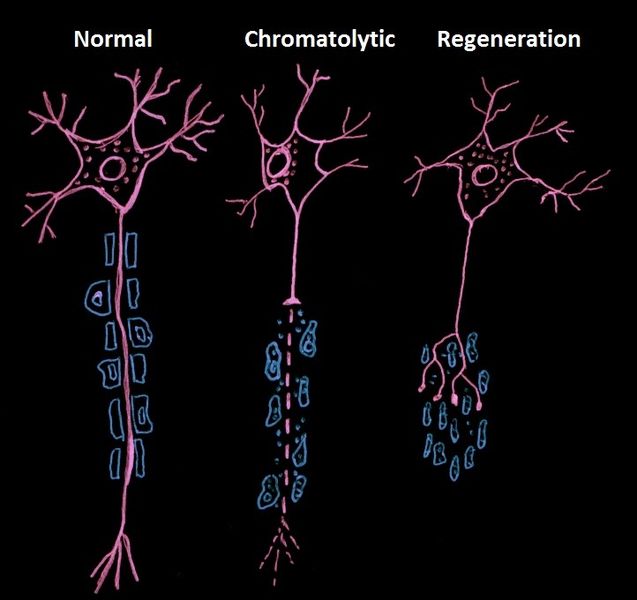
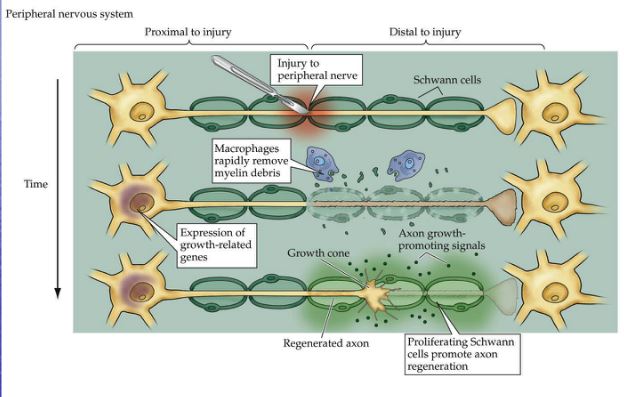
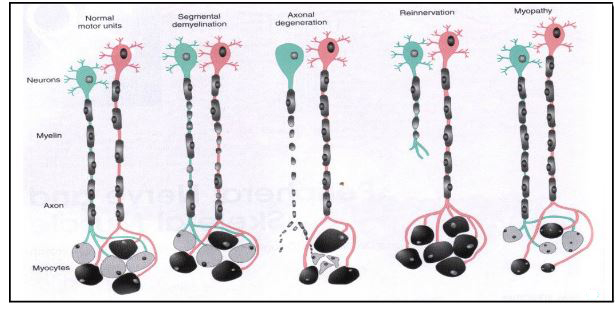
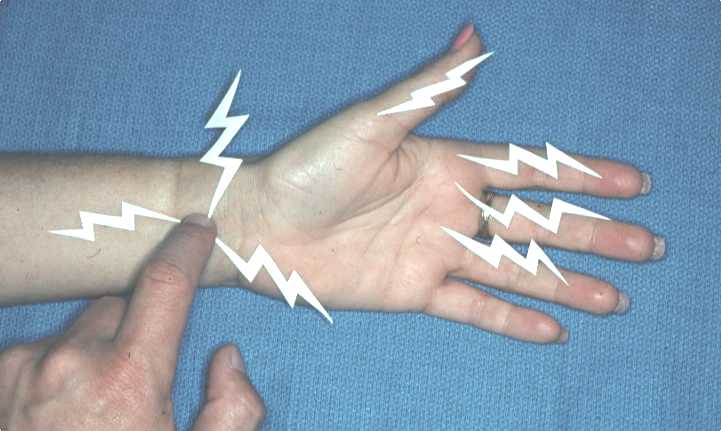
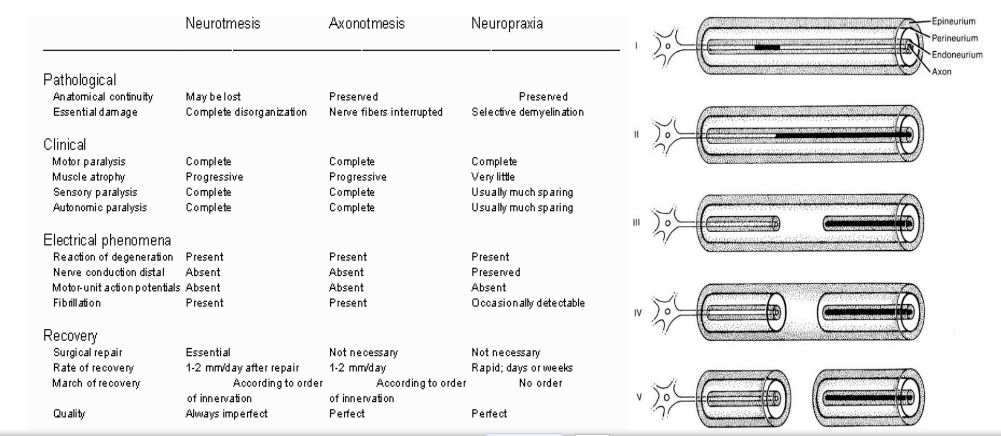
Nerve injury usually occurs as a result of pressure, blunt injury or transection, and the severity and duration of the symptoms depends on the degree of damage inflicted. The milder degrees of nerve injury produce transient symptoms without the effects of complete transection of the axon. Symptoms arising from pressure on nerves include weakness of the muscles that are innervated, and sensory symptoms of tinglings, numbness or lack of sensation. Neurapraxia is a condition where pressure on the nerve reduces bood flow and may cause some damage to myelin, resulting in a transient block of action potentials. The effects on nerve conduction are reversible and transient. Axonotmesis is more severe that neurapraxia., and causes conduction block in the axon. If the axon degenerates, time is needed for the axons to grow back through their endoneurial sheaths to reinnervate the muscle and sensory endings they had done originally. Neurotmesis is the most severe injury, with axons and the nerve sheath being severed. Axons develop growth cones but do not necessaily grow along their original fasciculi, and may reinnervate targets other than the original ones. |
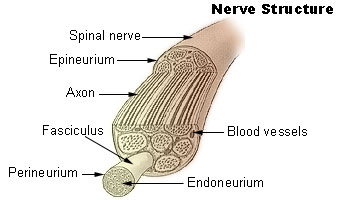
The diagram shows the structure of a peripheral nerve. A connective sheath, the epineurium, surrounds each spinal nerve, and the nerve fibres are arranged in bundles called fasciculi. Each fasciculus has a membrane around it (the perineurium) and each axon is supported by a tube of connective tissue - the endoneurium.
Neurones in the peripheral nervous system are able to regrow and reinnervate their taget organs after injury to their axons, whereas damage within the CNS is not normally associated with the ability to regenerate axons.
|
 * * |
|